The Legionella bacteria is endemic in cooling towers throughout the United States, according to a recent study by the Centers for Disease Control and Prevention (CDC).
The CDC tested water from 196 cooling towers in eight of nine continental U.S. climate regions, and 84 percent returned positive results for Legionella DNA, meaning the bacteria was either present or had been present at some point. Overall, investigators found live Legionella bacteria in 79 cooling towers – half of which had more than one type of Legionella – in most regions of the country.
Legionella bacteria is the cause of the respiratory illness Legionnaires’ disease, a severe – often lethal – form of pneumonia.
The CDC study is the first to illustrate how prevalent Legionella may be in cooling towers, which are known to be a prime culprit in Legionnaires’ disease outbreaks. In two recent and well-publicized outbreaks:
- Between August and September in 2016, one person died and 23 people were sickened in a Hopkins, MN, outbreak. Officials identified a Citrus Systems, Inc., cooling tower as the source.
- In 2015, contaminated cooling towers were responsible for the deaths of 12 and more than 120 others becoming infected with Legionnaires’ disease in the South Bronx, NY.
The CDC had previously announced a 286% increase in the number of reported Legionnaires’ cases in the U.S. between 2000 and 2014.

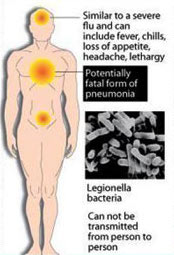 gionnaires’ disease diagnosed? The symptoms of Legionnaires’ disease look like other forms of pneumonia or even the flu, which is why so many cases go unreported. Early symptoms can include:
gionnaires’ disease diagnosed? The symptoms of Legionnaires’ disease look like other forms of pneumonia or even the flu, which is why so many cases go unreported. Early symptoms can include: