Another resident has taken ill with Legionnaires’ disease at the Illinois Veterans Home in Quincy (IVHQ), a month after two residents were sickened with the disease, according to a Nov. 28 news release from the Illinois Department of Health.
The illnesses come two years after a 2015 outbreak at the IVHQ in which 12 people died and 53 others were sickened.
The resident was diagnosed while being treated at a local hospital over the weekend and has since been released. One of the two individuals sickened last month died.
The IVHQ undertook a nearly $5 million, state-of-the-art rehabilitation of its water-treatment plant in summer 2016. There were four cases of Legionnaires’ disease at the facility in 2016, including three after the rehabbed plant was made operational.
Dave MacDonna, an Illinois Department of Veterans’ Affairs spokesperson, believes the spike in Legionnaires’ diagnoses could be due, in part, to the increase in testing for the pneumonia-like disease. Illinois experiences about 300 cases each year.
McDonna said the home was in a state of “high alert,” and any resident displaying symptoms is tested regularly and hospitalized if symptoms persist.
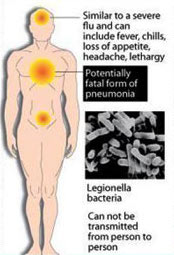
Legionnaires’ disease symptoms
Legionnaires’ disease looks like other forms of pneumonia or even flu, which is why so many cases go unreported every year. Early symptoms can include:
- chills
- fever, which can be 104 degrees or higher
- headaches
- loss of appetite
- muscle aches.
After the first few days, symptoms can worsen to include:
- chest pain when breathing, called pleuritic chest pain (due to inflamed lungs)
- confusion and agitation
- a cough, which may bring up mucus and blood
- diarrhea (about one-third of all cases result in gastrointestinal problems)
- nausea and vomiting
- shortness of breath.
The incubation period – the amount of time between contracting the bacteria and developing symptoms – is usually 2 to 10 days. However, it can be as much as 16 days.
Who is at risk?
Anyone can get the disease, but those at higher risk of infection include:
- people 50 or older
- current or former smokers
- heavy drinkers of alcohol
- people with chronic lung disease
- people with suppressed immune systems
- organ-transplant recipients
- people who are following specific drug protocols (corticosteroids, for example).
(Photo credit: Michael Kipley / Quincy Herald-Whig via The Associated Press)